Abstract
Young people living with long-term medical conditions growing into adulthood face significant challenges inherent in the necessary new-found autonomy and unprecedented responsibility for their health along with understanding the interfaces with adult health services. Data from the United Kingdom has found that amongst people living with Sickle cell disease (SCD), young adults aged 20-29 years have the highest rates of emergency hospital admissions. This is associated with a significant increase in mortality amongst patients with SCD of this age group.
It is well recognized that those who don't understand health information are less likely to seek out healthcare support appropriately and are more likely to have significant ill-health. Furnishing young people with the skills to improve their health literacy is therefore the cornerstone of any transition preparedness programme. Ready Steady Go (RSG) is a UK National Institute of Health and Care Excellence (NICE) endorsed generic transition programme that may be used to support children with long-term conditions. It comprehensively addresses the full range of issues for good transition and facilitates discussion in greater depth of any areas of need to support young people with chronic medical conditions so that they might more effectively manage the needs of their medical condition and navigate entry into adult life with confidence.
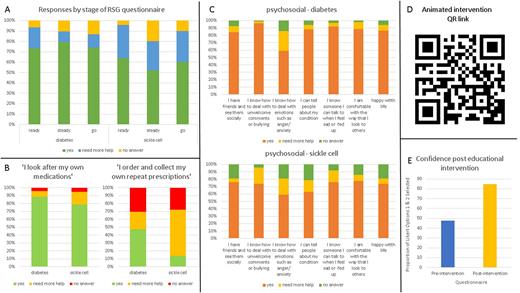
Data were compared between responses of 147 young people with chronic conditions transitioning to adult care at each of the Ready, Steady and Go timepoints. Age-appropriate questionnaires were offered as part of routine patient care and 4451 unique responses to each of the questions on the age-appropriate RSG questionnaires were obtained including responses related to knowledge and understanding of the condition, its treatment and the composition of the healthcare team, capacity for self-advocacy, assessment of understanding of general adolescent health issues including sexual health, exercise and diet, educational, independence and vocational domains, psychosocial aspects and the understanding of the concept of transitional care. Experience using these questionnaires in clinical practice has taught us that often the questions not answered are at least as informative as those answered as 'need more help' and are often areas with the highest need so we elected to include questions without a response in our evaluation.
Analysis revealed that at all stages the young people with SCD (n = 42) were significantly less likely to report confidence in important transition parameters compared to those living with other long-term conditions (n = 105) (figure A). This was most pronounced in questions that assessed knowledge and understanding of their medications and how they worked and ownership of taking their own medications without parental assistance (79.9% SCD vs 89.9% other chronic conditions) with low reported rates of requesting and picking up their own repeat prescriptions (13.9% SCD vs 47.4%) (figure B). Patients with SCD were more likely to report that they needed more help 'dealing with unwelcome comments or bullying' (26.1% SCD vs 3.5%) and less likely to 'feel happy with life' (73.8% SCD vs 86.4%) (figure C). They were also more likely to reply that they did not feel able to 'tell others of their condition' (36.8% SCD vs 11.8%) and were less likely to say that they were 'happy with the way they looked to others' (77.8% SCD vs 86.4%). Our data also suggested that their social support was less with 24% of respondents with SCD saying they did not 'know someone I can talk to when I feel sad or fed up' vs 8.3% of respondents with diabetes. 23.8% of young people with SCD reported they did not see friends outside of school vs 15.5% of young people with diabetes.
In response to these data, a bespoke, bite-sized, animated SCD transition education package was developed (figure D). It was offered to young people living with SCD peri-transition and demonstrated an uplift in confidence and understanding from 47.8% to 84.6% after engagement with the resource (figure E).
This data analysis and reflexive action research shows that there is a significant health literacy gap in young people with SCD transitioning to adult care, larger than that seen in young people with other chronic conditions and that targeted digital health education interventions are effective at increasing a young person's health literacy, engagement and confidence.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal